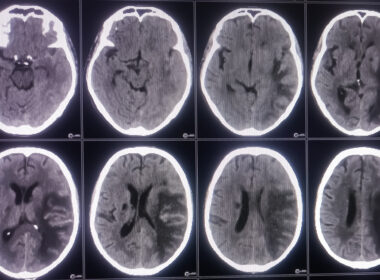
Pressure ulcers are just one of the many avoidable complications affecting thousands of people each year who enter nursing homes and hospitals for medical treatment or rehabilitation.
Pressure ulcers form when a person’s soft tissue is compressed between a bony prominence and an external surface for an extended period. It can be worsened by prolonged sustained pressure on specific body parts.
Pressure ulcers are bed sores when blood circulation cuts off from body parts due to excessive and prolonged pressure. If the skin has been damaged to the dermis level, but not further, that pressure ulcer is considered at the stage 2 level. The same applies to blisters that have already burst.
Etiology of Pressure Ulcers
Pressure ulcers are accepted as caused by three distinct tissue forces:
- Prolonged pressure: Most pressure is caused by bone pressure against an area. When this pressure exceeds the capillaries, this depletes the surrounding tissues of oxygen.
- Shear: These forces generally occur due to patients staying under the skin. At the same time, deep fascia and sprained skeletal muscle are pushed down, causing the vessel to collapse, causing tissue and ischemic damage.
- Friction: The friction forces are opposite the shear forces in nursing home residents with pressure ulcers.
Stages of Pressure Sores
Pressure sores are usually referred to as swollen beds. It occurs when someone sits on a sofa for longer than they are sleeping, and the body’s weight on a chair reduces blood flow. Pressure sores can be found in beds or wheelchairs. The four stages of pressure sores include:
- Stage 1 ulcers have not yet broken through the skin;
- Stage 2 ulcers have a break in the top two layers of skin;
- Stage 3 ulcers affect the top two layers of skin, as well as fatty tissue;
- Ulcers are deep wounds that may impact muscle, tendons, ligaments, and bone.
Accurate knowledge about these stages is vital in Recognizing and treating pressure sores, especially in the presence of suspected deep tissue injury or surrounding skin inflammation.
Description of Stage 2 Pressure Ulcers
These phases vary depending on the depth of the sore, which affects treatment. When grade 2 pressure ulcers are diagnosed at an early stage, it’s possible that these sores can be quickly healed. Unless you treat them, things can worsen. The sore will appear pinker when the tissue is negligible.
Stage 1
It was a mild phase. This sore only touches the upper skin surface.
Symptoms include:
- Itching and itchy skin may also be a common cause of pain. Often it feels different than the skin surrounding it;
- Redness of the skin. The area doesn’t light up immediately if the button is stopped pressing. So less blood reaches this location. If your skin is darker, it will be easier to spot discolored skin.
Stage 2 Pressure Ulcer
Pressure ulcers or decubitus ulcers are closed or open wounds resulting from an interruption in blood flow. The grade 2 pressure sore usually arises when sitting in a position and is often referred to by doctors as a bedsore if prolonged.
People who develop pressure ulcers in a chest area have mobility difficulties or are asleep.
Pressure ulcers are tissue necrosis characterized by tissue compressed by a bony prominence over a long time.
Stage 2 pressure ulcers can cause skin irritation but not deep into the dermis. This is a blister in which the wound has remained intact.
Symptoms of Stage 2 Pressure Ulcer
The base of a stage 2 pressure ulcer is red and shallow. Granulation tissue, slough, and eschar are absent, as is adipose (fat) and deeper tissues. Stage 2 pressure ulcers can also include intact or partially ruptured blisters caused by pressure. Partial-thickness skin loss with exposed dermis is familiar with stage 2 pressure ulcers.
It is important to remember that the definition of a stage 2 ulcer does not encompass erosion, ulceration, or blistering caused by factors other than pressure (such as skin tears, maceration, excoriation, etc.)
Symptoms of stage 2 bedsores are open wounds that have broken the epithelium’s upper layer. Stage 2 beds may be found in any area of the earth.
Generally, areas closer to bone are more vulnerable. Bedsores usually form around: Clear fluids or pus can be discharged into affected areas, and nearby skin will discolor.
The University of Maryland noted that patients who suffer from stage 2 Bedsores have significant pain. The pain may lessen when sores worsen but become harder to manage and cause serious complications.
Signs of Stage 2 Bed Sore
Bedsores in the second stage have penetrated the dermis but have not yet reached the fatty tissue beneath. The longer it takes and the more difficult it is to treat an open wound, the deeper it is.
Regular skin checks should be performed on people at risk of developing bedsores to detect sores before they progress past stage 2. The signs include:
- Intact or ruptured blister
- Irritated skin
- Pus or fluid
- Redness or discoloration
Bedsores are a severe medical problem that can cause death or limb loss in extreme cases. It is critical to detect a stage 2 wound as soon as possible. Neglected bedsores can lead to severe complications.
When an open wound gets infected, the bacteria can travel through the body and lodge themselves in the heart, blood vessels, or bones.
If you or a loved one has developed a bedsore in the second stage, you should seek medical attention immediately. A medical professional can determine the best course of action for treating bedsores.
Causes of Stage 2 Bed Sore
Bedsores or pressure injuries occur in the bloodstream that stops functioning correctly. Having to lie still and not get enough sleep reduces blood flow affecting surrounding tissues.
Stage 1 bedsores do not break the skin; however, sitting at the same place when the skin forms may tear the skin up and cause Stage 2 bedsores to develop.
A nursing home ill-tended may be associated with swollen feet or bed. A lack of training and understaffing may inhibit the ability of staff to accommodate resident mobility needs.
If stage one bedsores are not treated quickly or effectively, they may develop into them. At this time, bedsores have slipped through skin layers to form open blisters that usually cause irritation or discoloration.
Patients with mobility issues often risk bedsores (pressure ulcers).
Symptoms are asymptomatic, may result in life-threatening conditions if left untreated, and are rare for bedsores.
Proper treatment of aging adults is helpful in recovery. Stage 2 bedsores are signs that nursing homes have abused or neglected their staff or patients.
How to Get Rid of Pressure Blisters?
After changing the dressing on an open sore, rinse it with water or a saltwater (saline) solution. Applying a bandage to a wound. The bandage’s ability to retain moisture promotes faster wound healing. Also, it prevents moisture loss and acts as a barrier to prevent infection in the skin around it.
Prevention of Stage 2 Bed Sore
Stage 2 bedsores may be avoided when Stage One bedsores are diagnosed early. Frequent mobility can help prevent pressure sores from developing. This involves pulling pressure off bed sand and washing it, taking the bed off the floor, and asking the physician for help if the problem does not resolve within two to three days.
A family member could look for stage 1 bedsores at nursing homes when they visit the residents. Nursing homes can prevent setting two bedsores if they recognize symptoms or significant symptoms of stage 1 bedsores.
Residents who believe staff members do not understand their concerns can speak directly to their loved ones.
Guarantee a sufficient calorie and protein intake. Keep moving around and stretching as much as you already are.
The use of positioning aids is recommended to avoid excessive stress on bony protrusions. To avoid getting your hair sheared off in bed, keep your head as low as possible.
Complications From Stage 2 Bedsores
Several cases associated with bedsores have been described. Bedsores in Stage 2 can penetrate deep tissues, which causes Stage 3 & 4 sores. Late-stage pressure sores will take longer to heal, leading to serious health problems that can cause death.
It is a frequent complication in patients with pressure ulcers. If an ulcer progresses too quickly, the result is osteomyelitis or sinus infections, either superficial or connected with a deeper structure.
Several cases associated with bedsores include:
Infections
Bedsores exposed to bacterial and viral infections are often associated with swollen joints, headaches, mental fog, and heart rhythm. Conditions may cause disease of the skin and bone, which causes diseases like sepsis and osteomyelitis.
Additional health problems
The MSKTC concluded bedsores increased the risk for infections with urinary tracts, and the condition also increased the risk of amputation.
Grade 2 Pressure Sore Treatment
Nursing blister treatment is done by frequently repositioning the patient, employing pressure-relieving mattresses, and covering the ulcer with a dressing. Surgical intervention may be required on occasion. Seek professional medical advice from trusted doctors or nurses to learn more about treating pressure sores.
Stage 2 Bedsore Life Expectancy
Most patients with Stage 1 or Stage 2 bedsores can recover within 2-3 weeks when prompt treatment is applied. However, the prognosis worsens for those with Stage 3 or 4 bedsores. Emphasis should be placed on proper nutrition and hydration to support wound healing to get to a healed stage 2 pressure ulcer. The medical doctor might remove any dead tissue and prescribe antibiotics to fight infection if it progresses to stage 3.
Pressure Ulcer Risk Factors
There are many contributing factors. Intrinsic contributing factors include:
- Malnutrition
- Dehydration
- Impaired mobility
- Chronic conditions
- Impaired sensation
- Decreased LOC
- Infection
- Advanced age
- Steroid use
- Pressure ulcer present
External contributing factors include:
- Pressure
- Friction
- Moisture
- Incontinence
- Shear
Pressure Ulcer Management
A pressure ulcer management plan should include the following.
- The proper surface must be provided.
- Reposition every two hours in bed
- Use pillows or a specialized boot to take the weight off your heel.
- Reposition every hour when in a chair
- Use pillow between legs for side lying
- Stay away from the trochanter.
- To avoid injury, avoid using devices shaped like doughnuts.
It’s crucial to lessen friction and shear forces. When skin is dragged across a rough surface, a mechanical pressure called friction is exerted, and the interaction of gravity and friction causes a different mechanical force called shear.
Because of the force it applies perpendicular to the skin, blood vessels in the dermis and sub-dermis become angular and stretched, leading to thrombosis and cellular death.