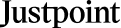
The term “brain death” has been used for more than 40 years to describe a complete cessation of all cognitive activity. A person would be deemed dead if their heart stopped beating, the standard method used before the mid-1940s. Pneumo-resuscitation and ventilation patients could “reversibly” recover from their condition despite their ability to escape life-support machines. This is why the Misdiagnosis of brain death is becoming an essential topic in the medical field.
What Is Brain Death
An artificial life support machine can cause brain death, known as “brain stem death,” when a person’s brain no longer functions. This makes brain death diagnosis,more complicated
To put it another way, this means being able to restore consciousness independently. Legally, a brain-dead individual has been declared dead. Due to their bodies’ inability to exist without mechanical life support, they have little prospect of recovery. Misdiagnosis of brain death or a delay in diagnosis accounts for one-third of all malpractice cases resulting in death or permanent disability.
Misdiagnosis in Mental Health
Medical or clinical professionals are often assumed to correctly understand a patient’s condition when consulted for treatment. They sometimes need to check or scan the entire brain.
On the other hand, misdiagnosis of being dead is more common than you might think, whether the diagnosis is incorrect or the professional cannot make one at all despite checking the entire brain. A correct diagnosis is not always straightforward, and misdiagnosis may prevent the actual condition from improving. As a result, it can worsen the underlying problem in many cases. To determine if a child is receiving adequate treatment, it is helpful to understand this common problem.
What Percentage of Brain Deaths Go Unrecognized?
Death rates following CPR are still high despite recent advances. Two-thirds of cardiac arrest patients hospitalized or placed in the intensive care unit (ICU) die before discharge. Deaths from hypoxic-ischaemic brain injury (WLST) are the most common cause of these tragedies, resulting from patients being actively removed from life-sustaining treatment due to their poor prognosis for survival of conditions related to the entire brain. However, in some resuscitated patients, hypoxic-ischemic brain injury can completely lose clinical brain function, i.e., brain death. Resuscitating patients who have suffered cardiac arrest and are unconscious should be thoroughly examined for signs of brain death. Sometimes the patients or their family members make various brain death accommodation requests during the investigation.
Can You Be Brain Dead and Still Function?
Legally, death by brain death is permitted. Because their heart is still beating and their chest continues to rise and fall with each breath from the ventilator, telling someone they have brain death can be confusing, leading to various brain death accommodation requests by the patient. Even if they are revived, they will never regain consciousness or be able to breathe for themselves again. If the medical profession cannot achieve rigorous, disciplined brain death testing by accepting official guidelines for determining brain death on a national scale, confusion and doubt may ensue, leading to erosion of public trust.
Brain Death as Opposed to Complete Unconsciousness
A person in a coma is utterly oblivious to their surroundings and unable to respond to anyone or anything around them. When a patient is unconscious but still conscious, they are said to be in a coma. Recovering after an injury is a complicated process that can take months or even years. Consent for brain death testing from surrogate decision-makers and brain death in the pregnant patient is one of the most challenging complications in brain death lawsuits.
Coma patients may have brain stem reactions, spontaneous breathing, and non-purposeful motor activity. There are three possible consequences of a coma: brain death, recovery of awareness, or evolution into a state of continuously depressed consciousness, such as a vegetative state. For brain death testing to be effective, the guidelines must be followed
It is impossible to donate organs, eyes, or tissue to someone.
Brain Death
When the brain shuts down, it’s game over. Brain activity does not exist at all. Swelling in the brain causes blood flow to stop, and without oxygen to the cells, the tissues die. It can’t be undone. After the death of brain tissue, nothing can be done to restore it to health.
The brain is responsible for a slew of complex neurological processes to keep vital bodily functions like blood pressure, heart rate, body temperature, hormones, and respiration under control. The body-brain is responsible for a slew of complex neurological processes to keep vital bodily functions like blood pressure, heart rate, body temperature, hormones, and respiration under control. The system shut down when a person dies of brain death. Once your brain stops working, you will not be able to breathe, your heart will not beat, and your body will cease to function. Intensive medical procedures (such as vented support) are necessary to sustain organ function, although they are just short-term solutions. This is precisely why brain death testing is important. Lack of compliance with the Brain Death Guidelines canlead to inaccurate determination of death.
How Do Doctors Test for Brain Death?
The three most significant clinical signs of brain death are irreversible and unresponsive convulsions and the absence of brain stem reflexes. Additional tests aren’t necessary if a comprehensive clinical examination, which includes testing for brain stem reflexes and apnea, is optimistic. Conclusive clinical findings or other ancillary tests must be present to confirm or diagnose a person’s brain death.
The following factors can be a risk factor for brain death:
- Someone must be completely unaware of their surroundings and unable to respond to external stimuli.
- A ventilator is required to keep a person’s heartbeat and breathing rate constant.
- Clear evidence must exist that a severe brain injury cannot be reversed.
If you or your loved one fall into the categories listed above, it is advisable to see a brain death misdiagnosis immediately.
Since you already know how brain death is diagnosed. Keep reading to learn more about how often brain death is misdiagnosis.
Why does Accurate Diagnosis of Brain Death Matter?
There are many functions of the brain stem, such as transmitting information about ourselves to the rest of the body and receiving information about ourselves from the rest, which is critical to the brain’s core functions. After a person’s brain has died, they cannot be conscious. Brain death (BD) should be the ultimate clinical expression of a brain catastrophe characterized by a complete and irreversible neurological stoppage, recognized by irreversible coma, absent brainstem reflexes, and apnea. An elevation of intracranial pressure manifests the most common pattern to a point beyond the mean arterial pressure. Hence, cerebral perfusion pressure falls, and, as a result, no net cerebral blood flow is present, leading to permanent cytotoxic injury of the intracranial neuronal tissue. A second mechanism is an intrinsic injury affecting the nervous tissue at a cellular level, leading to BD if extensive and ongoing. We review the methodology of diagnosing death based on finding any signs of death. The irreversible loss of cardio-circulatory and respiratory functions can cause death only when ischemia and anoxia are prolonged enough to produce irreversible destruction of the brain. The sign of such loss of brain functions, that is to say, BD diagnosis, are thoroughly reviewed. This is why it is essential to discuss the challenges of defining and diagnosing brain death. Adult brain death guidelines require a single brain death examination (with optional confirmation by another physician)
Can You Be Misdiagnosed as Brain Dead?
Comatose people do not respond to light or pain, and their sleep-wake cycle .circulatory and respiratory functions are disrupted. Patients placed in a “locked-in” state are awake and alert but unable to move or speak. They’re sharp, but they don’t show any signs of awareness that can be detected by medical science, such as MRI scans, like the Persistent Vegetative State (PVS). Patients may be misdiagnosed as “brain dead” if their doctors fail to order the necessary tests to determine whether or not they are aware of their condition and unable to communicate.
Individuals who have suffered severe brain injuries need to be accurately diagnosed to receive the best possible care and treatment. If a person is misdiagnosed, they may not receive the care and treatment they need to improve their quality of life. Patients who are conscious but whose life family members or doctors have turned off support systems may die due to the negligence of those in charge of their care. Non -compliance with brain death guidelines led to much medical malpractice in most health care institutions.
Is There a Difference Between Brain Dead and No Brain Activity?
The legal definition of brain death and inactivity states that As long as a person is not entirely brain-dead, they can still be kept alive in a modern intensive care unit with the help of artificial means. i.e., there is no activity in the brain. When the brain’s cells swell and die without receiving oxygen from the bloodstream, neurological death can then be undone. The end of brain cells is irreversible.
Why is Brain death permanent?
Despite being unconscious, a person’s brain elements are continuously active, and their condition could improve. Those who have been declared brain dead by the medical team due to lack of neurological function, o the other hand, are deemed to have lost all of their brain function and hence cannot be revived.
What Are the Long-Term Consequences, When Deprived of Oxygen?
Some of the long-term consequences of oxygen deprivation include a wide range of organ damage and problems. It’s possible that your child could experience long-term delays and issues due to their injuries and the sections of their body that were deprived of oxygen.
A brain injury caused by oxygen deprivation, known as hypoxia or anoxic brain injury, can have modest, short-term effects like dizziness or difficulty concentrating up to the severe and long-term vision, speech, and memory challenges,
Children can have life-altering medical issues and disabilities, and minor delays. Some of your child’s birth asphyxia-related issues may not become apparent until they reach specific developmental stages. It’s possible that you won’t know the long-term impacts on your child until they’re several months old or even until they start school.
Does a Brain Dead Person Have a Shelf Life?
Brain-dead people may theoretically be maintained alive for an extended period in suitable intensive care units, perhaps permanently, using ventilators,and blood pressure augmentation,
Is It Possible for Someone Who Has Lost Consciousness to Exhale on Their Own?
Reflexes are lost, and the person cannot breathe independently when they are “brain dead.” They are regarded as legally dead because they will never regain awareness or the ability to live on their own. As soon as a person loses the ability to function properly because of damage to the brain, their heart stops beating and dead.
Dead Brain Still Have a Beating Heart?
Spite despite higher brain processes, a person in a persistent vegetative state can maintain vital functions like heart rate and respiration thanks to their healthy brain stem. Even in a vegetative state, recovery is possible, but it will take time. This means that the person has died when the brain is no longer working.
What Is the Pre-brain Death Stage?
Constant coma, the absence of brain stem reflexes, and the inability to breathe alone are necessary circumstances for a person to be declared brain dead. breathe failure to get there on one’s own is An eye-opening verbal response and no movement of the patient’s limbs is a sign of coma.
Testing for Brain Death
Despite its conservative nature, brain death is only diagnosed when there is no question about the results. Sometimes it can be complicated due to the patient’s personal religious beliefs leading to problems with accepting brain death.
Doctors will run a battery of tests dead to see if the entire brain death patient has died. There is no response to verbal or visual commands; the patient is flaccid; the pupils are nonreactive and fixed; there are no oculocephalic, gag, or corneal responses; and the patient does not spontaneously breathe.
Before declaring brain death, many doctors request additional testing, even once the results of these tests are confirmed. For example, an electroencephalogram (EEG) or a cerebral blood flow (CBF) examination is a frequent diagnostic tool.
Electroencephalography (EEG) uses microvolts to detect brain voltage. If someone’s clothes have a static charge on them, the EEG will show an irregular pattern (a false positive). All of the affirmative responses show that the brain is working properly. Those in the most profound coma will exhibit EEG activity, while those who are dead will not.
A modest radioactive isotope is injected into the bloodstream to measure cerebral blood flow (CBF). The amount of blood flowing into the brain can be measured by placing a radioactivity counter over the subject’s head. The brain is considered dead if it is deprived of oxygen-rich blood. When cerebral flow testing comes back negative, it is foregone once the brain is dead.
Organ donation can be considered when a person’s brain death has been established and the exact moment of death has been recorded.
How Long Can Someone Remain on Life Support If They Show No Signs of Mental Activity?
A brain-dead individual will die in minutes once life support is removed because they will be unable to breathe independently. If a person is not brain-dead bu,t in a lifelong vegetative state, their life support system is most likely fluids and nourishment.
When Is It Appropriate to Declare Brain Dead?
The presence of three symptoms is necessary for brain death determination and diagnosis: chronic coma, the absence of brain-stem reflexes, and the inability to breathe independently. No movement of the patient’s limbs, no eye-opening, and verbal response are all signs of convulsion.
How Long Does It Take for Your Brain to Die from a Lack of Oxygen?
Coma and seizures are among the potentially fatal side effects of a lack of enough oxygen in the bloodstream. A person’s brain begins to die after ten minutes without oxygen. Death by the brain means the absence of any mental activity. The use of a mechanical ventilator, for example, is necessary to keep a person alive and breathing.
Several Diseases Can imitate Brain Death.
Brain death imitates
- Intoxication that is not recognized (e.g., tricyclics, lidocaine, baclofen, barbiturates, paralytics, anticholinergics, organophosphates);
- locked-in state of mind;
- Injury to the high C-spine.
- Hypothermia.
- GuilGillianre Syndrome is n its most advanced stage of manifestation.
Death: Isn’t It Time to Find a Uniform Definition?
A brain death diagnosis is nearly always confusing and overwhelming to family members. People who are declared brain dead by a court are deemed to have passed away because their condition is irreversible. Because their heart is still beating and their chest is still rising and falling with every breath from the ventilator, telling someone they have brain death can be confusing. But they will never regain consciousness or begin to breathe on their own. Sadly, they’ve already been buried. This is why brain death worldwide is considered dead, and there should be no confusion—brain death is Irreversible cessation of all functions of the entire brain, including the brain stem.
Another Brain Death Misdiagnosed Patient Saved Just in Time
This is an example of a story in which a hospital doctor misdiagnosed a man with brain death. This is why many people search in line for brain death recovery misdiagnosis.
A middle-aged African American went to a Clinic in Texas three times, claiming to be sick and suffering from vomiting and bleeding from his eye with a fever. The clinical diagnosis is food poisoning on all three of the occasions he was sent home. As his health worsened, he was rushed to the emergency room, where doctors did tests and discovered that he had a brain bleed, and they immediately put him on a ventilator. Over the previous week, he was admitted to another hospital, where he was declared brain-dead by physicians. Family members are fighting to keep him on the ventilator because they believe he will recover. He does not have any underlying health conditions or a history of substance misuse.
The brain death misdiagnosis victim came to JustPoint. Our medical experts listened to their stories and connected to a qualified attorney with a proven track record in similar cases. Our Legal team was able to help the victim get the compensation they deserve.
estimated settlement: $113,813
- conservative settlement: $111,581
- settlement offers:$119,809
Let’s Help you get the Compensation You deserve.
Conclusion
A person who is brain dead has been legally declared dead. Inability to survive without mechanical life support means that they have little hope of rehabilitation. To avoid confusion, it is best to leave the final diagnosis to the doctor in the event of a medical professional’s incorrect diagnosis of brain death. Don’t worry; Just Point is here to help. We’ll guide you through the legal process and ensure that you get the maximum compensation possible.